COLONOSCOPY | REASONS | PREPARATION | RECOVERY- Dr. Arun Aggawal
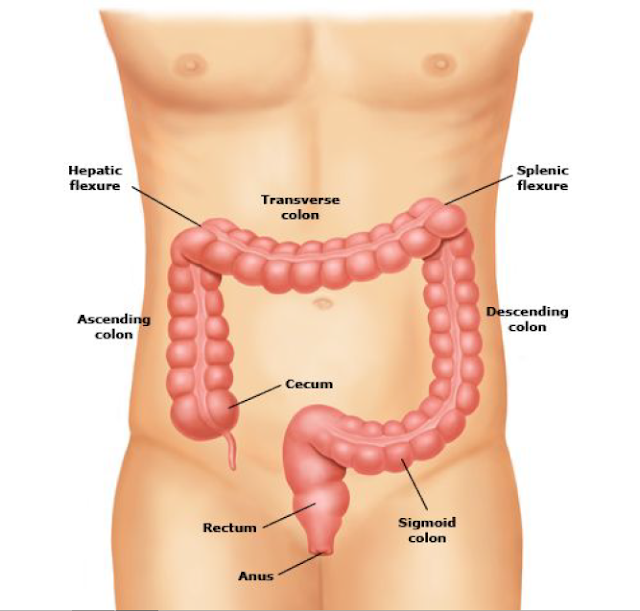
A colonoscopy is an exam of the lower part of the gastrointestinal tract, which is called the colon
or large intestine (bowel).
Colonoscopy is performed by inserting a device called a colonoscope into the anus and
advancing through the entire colon.
REASONS FOR COLONOSCOPY
The most common reasons for colonoscopy are:
● To screen for colon polyps (growths of tissue in the colon) or colon cancer
● Rectal bleeding
● A change in bowel habits, like persistent diarrhea
● Iron deficiency anemia (a decrease in blood count due to loss of iron)
● A family history of colon cancer
● A personal history of colon polyps or colon cancer
● Chronic, unexplained abdominal or rectal pain
● An abnormal x-ray exam, like a barium enema or CT scan
COLONOSCOPY PREPARATION
Before a colonoscopy, your colon must be completely cleaned out so that the doctor can see any
abnormal areas. This is vitally important to increase the chances that your doctor will identify
abnormalities in your colon. Your doctor's office will provide specific instructions about how you
should prepare for your colonoscopy.
You will need to avoid solid food for at least one day before the test. You should also drink
plenty of clear fluids on the day before the test. You can drink clear liquids (a liquid you can hold
up to the light and see through) up to several hours before your procedure, including:
● Water
● Clear broth (beef, chicken, or vegetable)
● Coffee or tea (without milk)
● Gelatin such as Jell-O (avoid red gelatin)
Avoid drinking red liquids. Your doctor may also ask you to avoid high fiber foods including
seeds and nuts for the week before the procedure.
To clean the colon, you will take a strong laxative and empty your bowels. You may be asked to
take the entire preparation the night before the test, or you may be asked to take it in two doses,
with the second dose taken four to six hours prior to the colonoscopy.
A commonly used preparation is a 4-liter (1 gallon) solution named Miralax or golytely. Some
doctors prefer citrate of magnesia (also called magnesium citrate), a 300 mL (10 ounces) bottle
that requires no mixing. Packets of powdered laxative are available that are mixed with a
smaller volume of water.
Drinking this solution may be the most unpleasant part of the exam. Watery diarrhea is the
desired result. This may occur shortly after drinking the solution or may be delayed for several
hours. The end result should be diarrhea that looks like urine. If you become nauseated or vomit
while drinking the solution, call your doctor for instructions. Tips that can help with nausea and
vomiting include temporarily stopping drinking the solution, walking around, and resuming
drinking at a slower pace.
Medicines — You can take most medicines right up to the day of the colonoscopy. Your doctor
should tell you what medicines to stop.
Transportation home — Most patients are given a sedative (a medicine to help you relax)
during the colonoscopy, so you will need someone to take you home after your test. Although
you will be awake by the time you go home, the sedative/anesthetic medicines cause changes
in reflexes and judgment that can interfere with your ability to make decisions, similar to the
effect of alcohol. You will not be able to drive home or go back to work after the examination if
you received sedation for the procedure. You should be able to return to work the next day.
THE COLONOSCOPY PROCEDURE
You will be given fluid and medicines through the IV line. With sedation/analgesia provided
during the colonoscopy, many people sleep during the test, while others are very relaxed,
comfortable, and generally not aware.
The colonoscope is a long black flexible tube, approximately the diameter of the index finger.
The doctor will gently pump air or carbon dioxide and sterile water or saline through the scope
into the colon to inflate it and allow the doctor to see the entire lining.
During the procedure, the doctor might take a biopsy (small pieces of tissue) or remove polyps.
Polyps are growths of tissue that can range in size from the tip of a pen to several inches. Most
polyps are benign (not cancerous). However, some polyps can become cancerous if allowed to
grow for a long time. Having a polyp removed does not hurt.
RECOVERY FROM COLONOSCOPY
After the colonoscopy, you will be observed in a recovery area, usually for about 30 to 60
minutes until the effects of the sedative medication wear off. The most common complaint after
colonoscopy is a feeling of bloating and gas cramps. You should pass gas and not feel
embarrassed doing this either during or after the procedure. This will relieve your feelings of
bloating and cramping. You may also feel groggy from the sedation medications. Most people
are able to eat normally after the test.
COLONOSCOPY COMPLICATIONS
Colonoscopy is a safe procedure, and complications are rare but can occur:
● Bleeding can occur from biopsies or the removal of polyps, but it is usually minimal and
can be controlled.
● The colonoscope can cause a tear or hole in the colon. This is a serious problem that
sometimes requires surgery to repair, but it does not happen commonly.
● It is possible to have side effects from the sedative medicines like nausea or vomiting.
● Although colonoscopy is the best test to examine the colon, it is possible for even the
most skilled doctors to miss or overlook an abnormal area in the colon.
You should call your doctor immediately if you have any of the following:
● Severe abdominal pain (not just gas cramps)
● A firm, bloated abdomen
● Vomiting
● Fever
● Rectal bleeding (greater than a couple of tablespoons [30 mL])
or large intestine (bowel).
Colonoscopy is performed by inserting a device called a colonoscope into the anus and
advancing through the entire colon.
REASONS FOR COLONOSCOPY
The most common reasons for colonoscopy are:
● To screen for colon polyps (growths of tissue in the colon) or colon cancer
● Rectal bleeding
● A change in bowel habits, like persistent diarrhea
● Iron deficiency anemia (a decrease in blood count due to loss of iron)
● A family history of colon cancer
● A personal history of colon polyps or colon cancer
● Chronic, unexplained abdominal or rectal pain
● An abnormal x-ray exam, like a barium enema or CT scan
COLONOSCOPY PREPARATION
Before a colonoscopy, your colon must be completely cleaned out so that the doctor can see any
abnormal areas. This is vitally important to increase the chances that your doctor will identify
abnormalities in your colon. Your doctor's office will provide specific instructions about how you
should prepare for your colonoscopy.
You will need to avoid solid food for at least one day before the test. You should also drink
plenty of clear fluids on the day before the test. You can drink clear liquids (a liquid you can hold
up to the light and see through) up to several hours before your procedure, including:
● Water
● Clear broth (beef, chicken, or vegetable)
● Coffee or tea (without milk)
● Gelatin such as Jell-O (avoid red gelatin)
Avoid drinking red liquids. Your doctor may also ask you to avoid high fiber foods including
seeds and nuts for the week before the procedure.
To clean the colon, you will take a strong laxative and empty your bowels. You may be asked to
take the entire preparation the night before the test, or you may be asked to take it in two doses,
with the second dose taken four to six hours prior to the colonoscopy.
A commonly used preparation is a 4-liter (1 gallon) solution named Miralax or golytely. Some
doctors prefer citrate of magnesia (also called magnesium citrate), a 300 mL (10 ounces) bottle
that requires no mixing. Packets of powdered laxative are available that are mixed with a
smaller volume of water.
Drinking this solution may be the most unpleasant part of the exam. Watery diarrhea is the
desired result. This may occur shortly after drinking the solution or may be delayed for several
hours. The end result should be diarrhea that looks like urine. If you become nauseated or vomit
while drinking the solution, call your doctor for instructions. Tips that can help with nausea and
vomiting include temporarily stopping drinking the solution, walking around, and resuming
drinking at a slower pace.
Medicines — You can take most medicines right up to the day of the colonoscopy. Your doctor
should tell you what medicines to stop.
Transportation home — Most patients are given a sedative (a medicine to help you relax)
during the colonoscopy, so you will need someone to take you home after your test. Although
you will be awake by the time you go home, the sedative/anesthetic medicines cause changes
in reflexes and judgment that can interfere with your ability to make decisions, similar to the
effect of alcohol. You will not be able to drive home or go back to work after the examination if
you received sedation for the procedure. You should be able to return to work the next day.
THE COLONOSCOPY PROCEDURE
You will be given fluid and medicines through the IV line. With sedation/analgesia provided
during the colonoscopy, many people sleep during the test, while others are very relaxed,
comfortable, and generally not aware.
The colonoscope is a long black flexible tube, approximately the diameter of the index finger.
The doctor will gently pump air or carbon dioxide and sterile water or saline through the scope
into the colon to inflate it and allow the doctor to see the entire lining.
During the procedure, the doctor might take a biopsy (small pieces of tissue) or remove polyps.
Polyps are growths of tissue that can range in size from the tip of a pen to several inches. Most
polyps are benign (not cancerous). However, some polyps can become cancerous if allowed to
grow for a long time. Having a polyp removed does not hurt.
RECOVERY FROM COLONOSCOPY
After the colonoscopy, you will be observed in a recovery area, usually for about 30 to 60
minutes until the effects of the sedative medication wear off. The most common complaint after
colonoscopy is a feeling of bloating and gas cramps. You should pass gas and not feel
embarrassed doing this either during or after the procedure. This will relieve your feelings of
bloating and cramping. You may also feel groggy from the sedation medications. Most people
are able to eat normally after the test.
COLONOSCOPY COMPLICATIONS
Colonoscopy is a safe procedure, and complications are rare but can occur:
● Bleeding can occur from biopsies or the removal of polyps, but it is usually minimal and
can be controlled.
● The colonoscope can cause a tear or hole in the colon. This is a serious problem that
sometimes requires surgery to repair, but it does not happen commonly.
● It is possible to have side effects from the sedative medicines like nausea or vomiting.
● Although colonoscopy is the best test to examine the colon, it is possible for even the
most skilled doctors to miss or overlook an abnormal area in the colon.
You should call your doctor immediately if you have any of the following:
● Severe abdominal pain (not just gas cramps)
● A firm, bloated abdomen
● Vomiting
● Fever
● Rectal bleeding (greater than a couple of tablespoons [30 mL])

Comments
Post a Comment